AANS Neurosurgeon : Features
Volume 24, Number 2, 2015
Screening for Chiari I Malformation
Karin M. Muraszko, MD, FAANS; Hugh J. L. Garton, MD, MHSc, FAANS; and Cormac O. Maher, MD, FAANSWho should be screened for Chiari Malformation Type I (CM)? It is impossible to have a “cookbook” standard that will apply to everyone. Consideration of symptomatology in relation to known associated conditions should lead the clinician to consideration for obtaining an MRI scan to diagnose a CM.
Diagnosing Chiari I Malformation
The symptoms associated with CM are, in many cases, non-specific and protean. Based on reviews of the extensive literature on CM, it is apparent that most neurological symptoms have at some point been associated with CM. The most common symptom is clearly headaches, but any number of brainstem and spinal cord associated symptoms has been attributed to CM in some patients. Many symptoms are, by themselves, commonly found in those with other neurological disorders or conditions. Therefore, the diagnosis of a symptomatic CM requires the clinician to actively include CM in the differential diagnosis, while also being careful to include other conditions that may mimic Chiari symptoms.
The decision to perform an MRI scan, particularly to rule out a CM, should start with a careful inventory of the patient’s symptoms and a thorough neurological exam. Headaches, the most common symptom associated with CM, can be associated with a variety of disorders. Headaches of a certain type and location, however, are particularly associated with CM. CM-type headaches are often short-lived, intense, located primarily in the occipital/sub-occipital/neck area and brought on with tussive episodes, such as sneezing or straining or during intensive physical activity. Lack of correlation with other common headache types, such as migraine or tension phenomena, may be important. Unfortunately, many patients have a mixed semiology to their headaches, making it difficult to determine the diagnosis with certainty. Left with a patient with severe, chronic or worsening headaches, the clinician must obtain an MRI of the head to rule out significant pathology.
Symptoms attributable to the brainstem and spinal cord are important to recognize. These symptoms include but are not limited to cranial nerve abnormalities, abnormal ocular movements, swallowing difficulties, coughing, speech or oral coordination disorders, central sleep apnea, dysmetria and ataxia. Spinal disorders, usually from a syrinx cavity, can include scoliosis, numbness or weakness in arms or legs, dysesthesias, coordination disorders, back pain and, more rarely, bladder or bowel dysfunction.
What Causes CM?
The origin of CM is an intensely debated issue. Multiple conditions can lead to the development of a CM appearance on imaging. Our current imaging definition of CM in the MRI era focuses on low cerebellar tonsil position. It is important to rule out hydrocephalus or an underlying tumor. In some cases, CM may be secondary to a variety of disorders that lead to bony abnormalities, such as calcium metabolism abnormalities, cranial suture synostosis, achondroplasia or disorders that can affect intracranial pressures, such as pseudotumor cerebri or intracranial hypotension. Associated soft tissues disorders, such as Ehler Danlos, and other connective tissue disorders can lead to settling and instability, resulting in disturbances at the foramen magnum, which can be characterized as CM-type problems.
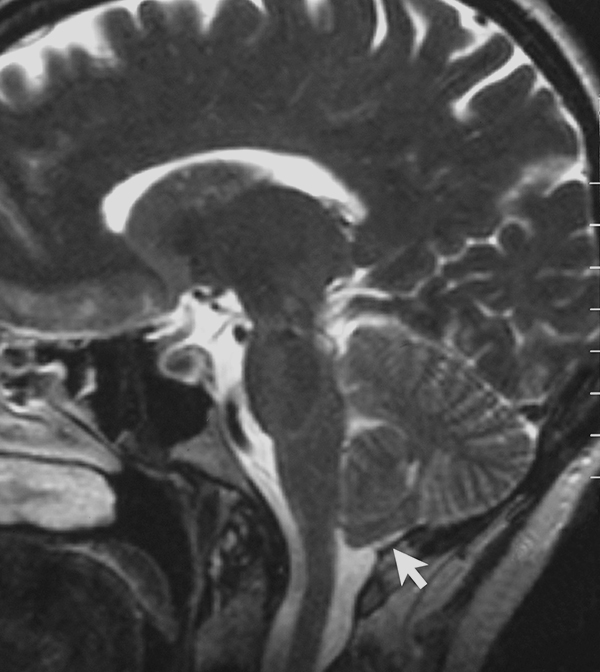 A T2-weighted sagittal MRI scan, from a patient with Chiari-like symptomatology, demonstrating tonsillar herniation less than 3 mm. Photo courtesy of Raymond F. Sekula Jr., MD, FAANS; Peter J. Jannetta, MD, DSc, FAANS(L); Kenneth F. Casey, MD; Edward M. Marchan, MD; L. Kathleen Sekula, PhD, APRN, FAAN; and Christine S. McCrady, Esq.
A T2-weighted sagittal MRI scan, from a patient with Chiari-like symptomatology, demonstrating tonsillar herniation less than 3 mm. Photo courtesy of Raymond F. Sekula Jr., MD, FAANS; Peter J. Jannetta, MD, DSc, FAANS(L); Kenneth F. Casey, MD; Edward M. Marchan, MD; L. Kathleen Sekula, PhD, APRN, FAAN; and Christine S. McCrady, Esq.
The dimensions and volume of the posterior fossa in families affected with CM suggests aspects of the association of genetic predisposition to CM. There are multiple reports of associated family members and twins having symptomatic CMs. The focus on a genetic origin to CM, however, may underestimate the diversity of abnormalities that may lead to the formation of a CM. An understanding of this diversity is crucial, particularly in decision-making with respect to treatment options.
Development of CM in individuals with previously normal neuroimaging suggests the fact that some cases of CM arise secondary to dynamic changes in the central nervous system. Our understanding of the diverse origin of CM is improving, and will likely result in further substratification of CM as not a single entity, but the reflection of a variety of disorders, all of which result in changes in dynamics at the foramen magnum.
Treatment Decisions in Neurosurgical Practice
In practice, the decision for screening a patient with neuroimaging often falls to a primary care physician or neurologist. As neurosurgeons, we have the luxury of most often seeing the patient after the screening decision has been made and a positive finding has been obtained. Neurosurgeons are, therefore, more often presented with a treatment decision rather than a screening decision. It is important that we recognize that the definition of CM by our radiology colleagues does not necessarily correlate with a need for surgical intervention, but demands of us an understanding of possible origins of the radiologic findings and understanding of their significance to the patient’s symptoms and neurological exam.
 Karin M. Muraszko, MD, FAANS, is the chair of and the Julian T. Hoff, M.D. Professor of neurological surgery at the University of Michigan (U-M). Hugh J. L. Garton, MD, MHSc, FAANS, is the Richard C. Schneider Professor of neurosurgery at U-M. Cormac O. Maher, MD, FAANS, is an associate professor of neurological surgery at U-M. All three physicians are pediatric neurosurgeons practicing at the University of Michigan Medical Center and C.S. Mott Children’s Hospital in Ann Arbor, Mich. The authors reported no conflicts for disclosure.
Karin M. Muraszko, MD, FAANS, is the chair of and the Julian T. Hoff, M.D. Professor of neurological surgery at the University of Michigan (U-M). Hugh J. L. Garton, MD, MHSc, FAANS, is the Richard C. Schneider Professor of neurosurgery at U-M. Cormac O. Maher, MD, FAANS, is an associate professor of neurological surgery at U-M. All three physicians are pediatric neurosurgeons practicing at the University of Michigan Medical Center and C.S. Mott Children’s Hospital in Ann Arbor, Mich. The authors reported no conflicts for disclosure.