AANS Neurosurgeon : Features
Volume 24, Number 2, 2015
Is It Real?
Deborah L. Benzil, MD, FAANS
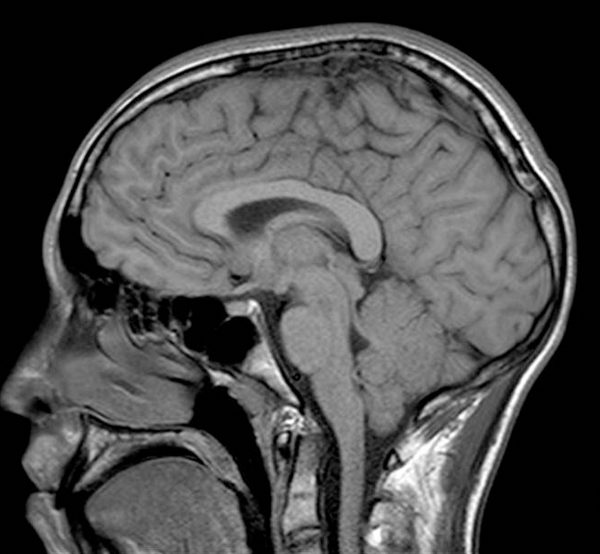
Historically, many neurosurgical diagnoses only became known under extreme conditions. However, with technological advances and our ability to easily, safely and noninvasively look inside the brain and spine, the incidence of many of these same entities has increased dramatically. Moreover, the connection between the findings and the presenting symptoms can be unclear. Frequently, neurosurgeons encounter desperate patients in their office who have spent anxious hours searching the Internet about a “diagnosis” they have been given, acquiring a great deal of information that may have little or no relevance to their specific situation. Unfortunately, neurosurgeons too often have limited hard data to determine how best to treat such patients — what additional testing might be useful, what statistics about prognosis actually apply, how to follow these patients radiographically or how to best advise them.
Addressing Incidental Findings
Just this week, my neurosurgical office was asked to evaluate the following patients on an urgent basis:
- A 16-year-old female neurologically intact with ADHD, chronic headaches, neck and back pain, and anxiety disorder who was found to have a 1-2 mm syrinx versus expanded central canal at C5-6
- A 17-year-old male with a sports-related head injury/concussion now asymptomatic but found to have a 2 mm “Chiari malformation”
- A 48-year-old woman with migraines since age 13 (non-smoker with no family history) seeing a new neurologist who ordered an MRI that was interpreted as having a 2 mm posterior communicating artery aneurysm or infundibulum
- A 34-year-old male with “ice-pick” headaches noted to have a 9 mm, non-enhancing, smooth-walled pineal cyst
Few neurosurgeons I know have any problem seeing these patients to reassure them — and often their families — about obvious incidental findings. However, they represent a challenge on many levels. The current challenges of health-care reform and the push to value further complicates the care of these patients. A real-life example can illustrate many of these issues.
Case Description and Subsequent Questions
A 62-year-old male presents to his primary physician with dizziness. The symptoms had an abrupt onset with no other associated neurological or systemic problems. The patient has a history of hypertension and high cholesterol, is treated for benign prostatic hyperplasia (BPH), formerly smoked with a 40-year pack history (he quit five years ago), and alcohol consumption of two glasses of wine a night. Before any formal ENT evaluation, a brain MRI was done, demonstrating a 2 mm enhancing mass in the right internal auditory canal (IAC) consistent with a small acoustic neuroma. Subsequent hearing tests were age-appropriate.
The first question to ask is whether this very small lesion (which would not have been visible on CT or on many early-generation MRI scans) has any relation to the symptoms? Most would conclude there is no association.
The next question is, does this acoustic neuroma require intervention? Fortunately, for this specific incidental finding, there are some good longitudinal studies (though none that include tumors this small) that demonstrate not all acoustic neuromas enlarge. One might conclude, therefore, that as it is asymptomatic, it requires no treatment. However, since many consider stereotactic radiosurgery to be a noninvasive, safe treatment this intervention may be offered. Is this an appropriate use of health-care resources? Are the small but real risks of such an intervention really represented to the patient? Are competitive (i.e. drive for RVU production or a successful radiosurgical program) forces a driving factor? Whatever the motivations, if this patient were unaware of this very small acoustic neuroma because technology was less advanced, these questions would never arise.
Following this inquiry, if no treatment is recommended at present, what follow-up should be recommended? MRIs are expensive tests. While the price varies widely across regions, facilities and based on insurance, there is both the facility (technical fee) and the radiologist fee (for interpretation) that starts around $3,000 and can range up to $8,000. One population study demonstrated an increased incidence of acoustic neuromas from 11.5/1 million to 17.4/million (pre-1996 versus post-1996). Applying this data to the U.S. population, that represents a $6.3 million expenditure for a single follow-up MRI for the technology-discovered acoustic neuromas. Is a single follow-up MRI at three months indicated? If unchanged, how often should follow up be done? Clearly, the costs of regular, long-term follow up can mount without a clear idea of how likely future intervention may be needed.
Considerations
All discussions of value should also consider the critical component of time, an increasingly valuable commodity for physicians as the push to efficiency and productivity takes hold. The time necessary for a neurosurgeon to clarify the real information about such an incidental finding is significant because the overwhelming available information relates to a prior era of neurosurgical diagnosis. In comparison, the average size of an acoustic neuroma has declined from just under 4cm several decades ago to under 1cm today.
In this issue, we try to address at least some of the questions raised by our current technological ability to peer inside of the nervous system. Right now, the findings often raise more questions than they answer. Data registries, such as NeuroPoint Alliance’s National Neurosurgery Quality and Outcomes Database (N2QOD) and electronic health record (EHR) systems that allow comprehensive, longitudinal study of these patients, will enable neurosurgeons to better provide the right care, for the right patient, at the right time in the future.
 Deborah L. Benzil, MD, FAANS, is a neurosurgeon with the Mount Kisco Medical Group (MKMG) in New York. On faculty at Columbia University in the department of neurosurgery, she also is director of restorative neurosurgery at Putnam Hospital Center in Carmel, N.Y. In addition, Dr. Benzil is a director-at-large on the American Association of Neurological Surgeons (AANS) board of directors, the immediate past chair of the Council of State Neurosurgical Societies and the associate editor of AANS Neurosurgeon. The author reported no conflicts for disclosure.
Deborah L. Benzil, MD, FAANS, is a neurosurgeon with the Mount Kisco Medical Group (MKMG) in New York. On faculty at Columbia University in the department of neurosurgery, she also is director of restorative neurosurgery at Putnam Hospital Center in Carmel, N.Y. In addition, Dr. Benzil is a director-at-large on the American Association of Neurological Surgeons (AANS) board of directors, the immediate past chair of the Council of State Neurosurgical Societies and the associate editor of AANS Neurosurgeon. The author reported no conflicts for disclosure.
One Comment
Comment on this Article
We welcome thoughtful comments from readers. Please comply with our guidelines.


It might be helpful to know if there was any nystagmus present or any difference in vestibular function tests of the right and left ear before deciding that the small tumor was not the cause of the “dizziness” or whether the dizziness was true vertigo. Also how bad and long lasting was the “dizziness” or vertigo. If only a short nonrecurring episode then only followup would be indicated. If over the next year recurring episodes of vertigo or progressive loss of hearing in one ear occurred indicating a more rapid growth of tumor and an indication for followup MRI. If this is not vertigo but dizziness or meuniere’s syndrome or related to his hypertension suitable treatment for the correct diagnosis should be done.
Report this comment