AANS Neurosurgeon : Features
Volume 24, Number 2, 2015
Defining the Appropriate: When to Screen Patients with Positive Family History of Aneurysmal SAH
Amir R. Dehdashti, MDWhat is the appropriate screening in patients with positive family history of aneurysmal subarachnoid hemorrhage? Despite documented evidence of higher risk of subarachnoid hemorrhage (SAH) in individuals with positive family history of aneurysm, the overall screening, management and counseling is not uniform.
Assessing Risk Factors
The first determinant factor is to identify who is the individual at risk. Only individuals with two or more first-degree relatives who have had aneurysmal SAH (or unruptured intracranial aneurysms), have an increased risk of aneurysms and aneurysmal SAH. Any description beyond this would not fit the criteria for screening in the context of positive family history.
The decision as to whether to screen for intracranial aneurysms should take into account several factors, including the frequency and natural history of intracranial aneurysms, the cost of screening, the treatment options, the patient’s age, co-morbidities and inevitable psychosocial impact of diagnosing an aneurysm.
When There’s a Family History
The risk of rupture of an incidental intracranial aneurysm is estimated at about 0.5-1 percent per year if the aneurysm is about, or more than, 5 mm in diameter. In a recent study, however, 65 percent of ruptured aneurysms were less than 5 mm in diameter. The prevalence of intracranial aneurysm is about 2 percent in the general population, and 4 percent in individuals with one affected first-degree family member. Individuals with positive family history (at least two affected first-degree relatives) have a risk of 8 to 10 percent of harboring intracranial aneurysms, and if they do, the risk of rupture is significantly higher than the known natural history of sporadic aneurysm, according to the International Study of Unruptured Intracranial Aneurysms (ISUIA) (up to 17-times higher with a matched distribution of size and location compared to sporadic aneurysms). Also, the outcome of SAH tends to be worse in the familial SAH context. The risk of having an intracranial aneurysm increases to 20 percent in high-risk individuals with two first-degree relatives and history of hypertension and smoking. Aneurysm multiplicity and MCA location is more common in familial intracranial aneurysms.
The familial occurrence of aneurysm has prompted several genetic research studies, and a potential linkage of familial intracranial aneurysms and chromosomes 4, 7, 8p22 and 12 have been identified. Recently, ADAMTS15 gene was considered a candidate gene for intracranial aneurysms.
Considerations for Screening
Overall, the indisputable risk factors for intracranial aneurysms are female sex, older age, positive family history and adult polycystic kidney disease (APCKD). Aneurysms are found in 10 to 13 percent of patients with polycystic kidney disease, which is clearly few times more frequent than the general population. The risk of SAH is, however, not much different in APCKD, compared to sporadic aneurysm, based on a recent 20-year follow-up study of 38 patients. Therefore, a routine screening for the population of APCKD is not recommended if the first screening’s imaging is negative for aneurysm.
In contrast, for familial aneurysms, the yield of long-term screening is substantial, even after more than a decade of follow-up and previous negative screens. It is suggested that these individuals have long-term serial screening despite initial negative screening, bearing in mind that the risk of aneurysmal SAH within screening interval is not eliminated.
The psychosocial effects of aneurysm screenings are often underrepresented. Close to half of patients who screened positive for an intracranial aneurysm may reduce their work or have changes in their self-esteem. Some patients might experience reduced quality of life after a positive screening, and in some individuals, the financial burden of such a finding is significant.
Case: 44-Year-Old Woman With Positive Family History
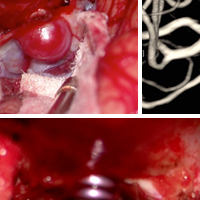
This 44-year-old woman with positive family history, identified on screening, was completely asymptomatic. Because of her young age, positive family history and, furthermore, history of hypertension, treatment was recommended. A 9 mm left ophthalmic artery aneurysm was treated by surgical clipping.
 Image 1: Left ophthalmic aneurysm on 3D angiogram. Image 2: Surgical exposure before anterior clinoidectomy. Image 3: After anterior clinoidectomy. Image 4: After clipping. Image 5: Post-operative angiogram.
Image 1: Left ophthalmic aneurysm on 3D angiogram. Image 2: Surgical exposure before anterior clinoidectomy. Image 3: After anterior clinoidectomy. Image 4: After clipping. Image 5: Post-operative angiogram.
The preferred screening modality is a 3T magnetic resonance angiography (MRA), which offers a very high sensitivity and specificity (98% and 94%, respectively). Once an aneurysm is diagnosed, a CT angiography (CTA) could be planned to better clarify the angio-anatomy of the aneurysm. However, CTA should not be the first screening modality, due to both radiation and contrast injection. The age at which the screening should begin is unknown. Siblings tend to present with SAH in the same decade. Similarly, aneurysms tend to rupture within the same decade in the member of same family. An anatomical vulnerability has also been identified in familial intracranial aneurysms with ICA territory, MCA territory and vertebrobasilar system distribution in this population. Given that intracranial aneurysms are uncommon before the age of 18, it is recommended to start screening children of high-risk families from age 18, but because of the absence of consensus on the exact age to start screening, it is not unreasonable to have the first screening even before the age of 18 (e.g >16 year old). Screening of individuals older than 75, or those with limited life expectancy, is not recommended.
Weighing the Risks and Benefits of Screening
Outside the true definition of family history of intracranial aneurysms, screening could be considered for individuals with only one first-degree relative and aneurysmal SAH, if two or three of the following risk factors are present: female sex, smoking, hypertension, APCKD and relatives of patient with multiple aneurysms and young age.
Despite strong evidence in favor of screening high-risk individuals, the physician should discuss the risks and benefits of screening, the implications of any incidental findings and the impact of those findings on patients’ quality of life, future potential treatments and risks associated with treatment. Screening with the appropriate indication has proven to be cost-effective in the setting of familial intracranial aneurysms. MRA screening of individuals at risk (two first-degree relatives with SAH or intracranial aneurysms) between the ages of 18 and 75, every five-to-seven years, provides a cost-effectiveness threshold of about $30,000/quality-adjusted life year and should be strongly considered and advised.
 Amir R. Dehdashti, MD, is a staff neurosurgeon and director of cerebrovascular neurosurgery research at Cushing Neuroscience Institute. Dr. Dehdashti is also an associate professor of neurosurgery at Hofstra Northshore LIJ School of Medicine, as well as an investigator at Feinstein Institute for Medical Research. The author reported no conflicts for disclosure.
Amir R. Dehdashti, MD, is a staff neurosurgeon and director of cerebrovascular neurosurgery research at Cushing Neuroscience Institute. Dr. Dehdashti is also an associate professor of neurosurgery at Hofstra Northshore LIJ School of Medicine, as well as an investigator at Feinstein Institute for Medical Research. The author reported no conflicts for disclosure.